According to a 2024 study by the National Center for Healthcare Workforce Analysis, there is a significant shortage of primary care physicians in the U.S., and conditions are only expected to deteriorate. The study shows “a projected shortage of 87,150 full-time equivalent (FTE) primary care physicians by 2037, which will be particularly acute in nonmetro areas.” This shortage has been exacerbated by the fact that an increasing number of MDs are choosing specializations over general internal medicine careers to earn higher salaries.
More Physician Assistants Programs Are Needed
As a result of the physician shortage, Physician Assistants and Nurse Practitioners now provide approximately one quarter of all primary care visits for American patients. The National Commission on Certification of Physician Assistants reported that the number of PAs in the U.S. increased by more than 6% from 2023-24, with an increase of 27% over the last five years. As of May 2025, the median salary has increased significantly. According to the American Academy of Physician Associates (AAPA), the median compensation for PAs “across all earning types” jumped to $134,000, up 5.5 percent from 2023, when the median salary was approximately $127,000.
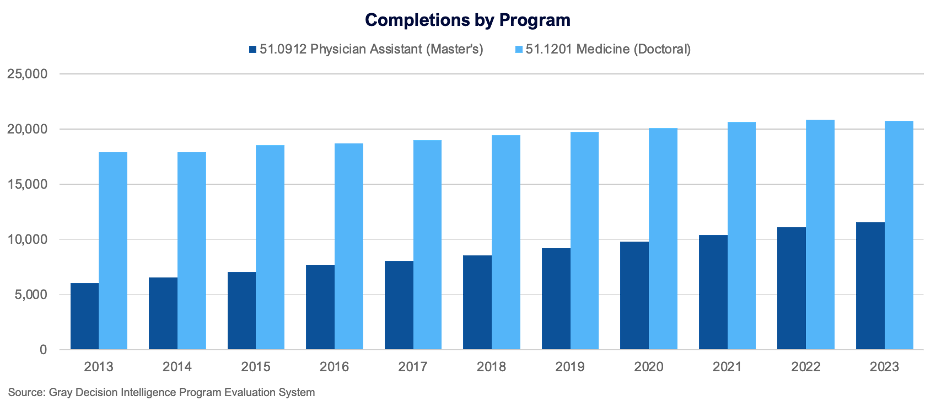
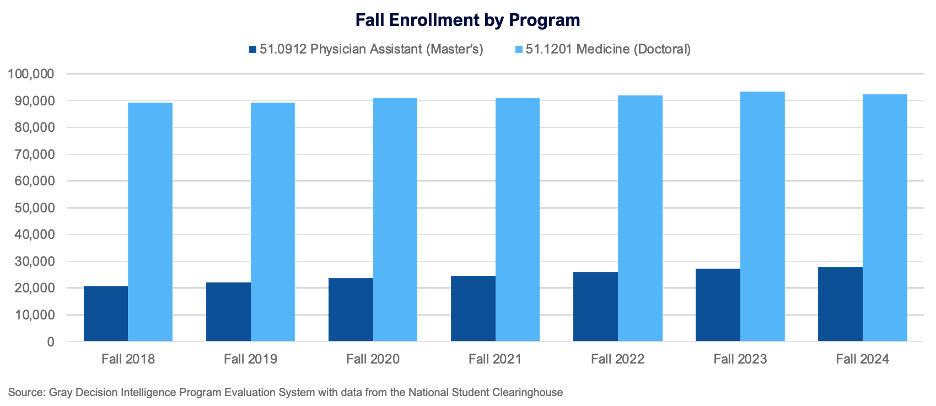
Are more future medical professionals considering the PA path as an alternative to the traditional MD path? It certainly appears that way. Recent enrollment and completions data for Physician Assistant master’s programs show a distinct upward trend. While MD programs still graduate more students each year, PA programs are growing faster.
Physician Assistant program completions jumped 91 percent from 2013 to 2023, compared to 16 percent growth in MD program completions.
 Similarly, enrollment in PA programs is growing faster than enrollment in MD programs. From fall 2018 to fall 2024, PA enrollment increased by 34 percent compared to a three percent growth for MD programs.
Similarly, enrollment in PA programs is growing faster than enrollment in MD programs. From fall 2018 to fall 2024, PA enrollment increased by 34 percent compared to a three percent growth for MD programs.
Many institutions have benefited from the rise in demand for PAs and PA programs. In 2013, 128 colleges and universities reported completions of PA programs; by 2023, that number had jumped to 243, a net change of 115 new entrants. Yet even as the number of schools offering the program grew, the average program size remained stable at 47 completions per campus, which suggests the market is not saturated and demand remains strong.
PA vs MD: Key Differences
Physician Assistant master’s programs were created in the 1960s to address a growing shortage of primary care providers. Duke University introduced the first PA master’s program in 1965. Confronted with the growing awareness of an increasingly unhealthy population, PA programs endeavored to shore up some gaps in the U.S. healthcare system.
Physician Assistant programs are usually two to three years in length, followed by 2,000 hours of supervised clinical practice. Prerequisites for PA Master’s candidates include prior (paid) healthcare experience. By contrast, it takes a minimum of seven years (post-undergraduate degree) to complete an MD track, which consists of four years of medical school, followed by three to seven years of rotation. In order to practice medicine, following completion of their respective medical programs, both MDs and PAs must pass comprehensive exams.
One significant difference between the two is that physician assistants cannot practice independently. They must be under the supervision of an MD, which allows them to gain practical experience on the job. Since PAs are not required to choose a specialty, they can practice across a broader swath of medicine.
PAs can perform many of the same aspects of patient care as MDs; they conduct exams, diagnose conditions, run and interpret diagnostic testing, and prescribe medications, among other things.
PAs often work 40 hours or more per week, but they are more likely to be on a regular “9 to 5” schedule than their MD colleagues. A PA career also offers opportunities for mid-career shifts and lateral flexibility. This more attractive work/life balance, and shorter pathway to the workforce, may be a deciding factor for future healthcare professionals choosing to pursue the PA path.
Will Patient Appreciation Lead to Program Growth?
Now that more patients in the U.S. are seeing PAs, a positive picture of public perception of the PA as a source of primary care has emerged. The 2023 Harris Poll showed that the majority of patients who see PAs report feeling confident in the quality of care they received, and are likely to keep seeing a PA as their primary care provider. Patients say they often feel less rushed at appointments, and appreciate the fact that they can get an appointment in a timely manner. These factors lead patients to feel less overwhelmed by the prospect of navigating the healthcare system. This is especially important in rural areas where care is often hard to find. Physician assistants can provide care in areas like telehealth, gynecology, dermatology, and behavioral and mental health, which are often in short supply for underserved populations.
PA programs provide an attractive alternative for students interested in medical careers who cannot or choose not to pursue an MD degree. They have also been an important source of growth for many colleges and universities. Faced with the reality of treating an aging and sicker American population, PA programs are providing a path back to wellness for the state of primary care in the U.S.
To explore this program for your region, contact us for a free chat.